Identifying care gaps along the HIV treatment failure cascade: A multistate analysis of viral load monitoring, re-suppression, and regimen switches in Zambia
An article in PLoS Medicine, published September 3, 2025.
Authors: Kombatende Sikombe, Noelle Le Tourneau, Brian Rice, Jake M. Pry, Sandra Simbeza, Laura K. Beres, Anjali Sharma, Njekwa Mukamba, Alison Wringe, James R. Hargreaves, Jacob Mutale, Carolyn Bolton Moore, Izukanji Sikazwe, Elvin Geng, Aaloke Mody
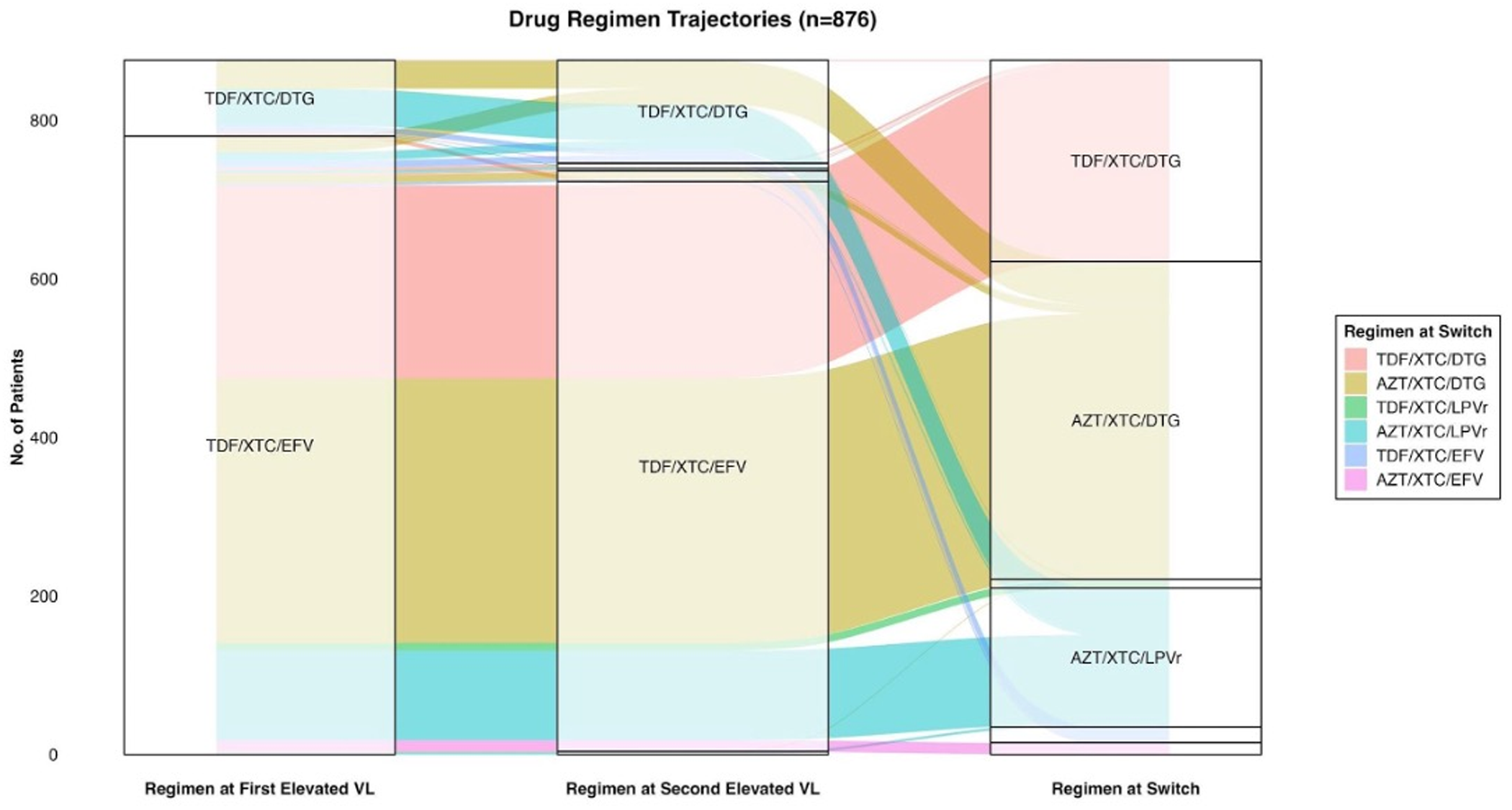
Figure: An illustration of the common regimen transitions among 876 study participants from the time of the first elevated viral load to the second elevated viral load and eventual switch (from referenced paper).
This study investigates the gaps in care following treatment failure among people living with HIV in Zambia, particularly focusing on viral load monitoring, re-suppression rates, and regimen switches. Data was collected from clinics in Lusaka between August 2019 and November 2021. Researchers looked at adults who had been on HIV treatment for over six months and had a high viral load.
Key findings:
Clinic Visits: 72% of patients returned to the clinic within six months after their viral load was found to be high.
Repeat Tests: 70% had their viral load checked again after one year, but some came back without getting another test.
Treatment Breaks: 17% stopped treatment for a while.
Getting Better: Among those who got another test, 85% on a newer type of medicine (TLD) got their viral load under control, compared to 58% on an older type (TLE).
Changing Medicines: For patients who needed to switch to a different medicine because their treatment wasn't working:
Only about 28% on TLD and 67% on TLE switched medicines within a year.
Some had an additional test before switching – those who had an additional test and switched had better outcomes.
Gaps in Care: The study found many delays and missed opportunities, like not having follow-up tests or waiting too long to switch medicines.
To improve HIV treatment, both patients and healthcare systems need to act faster and work better together. This means helping patients stay on track, regularly checking their viral load, and quickly switching medicines when needed. By doing this, people living with HIV can have better health outcomes.